Enlarged blood vessels around your esophagus are called varices. If they rupture, it may be fatal. Variceal banding is a procedure that prevents and treats these ruptures.
Advanced liver conditions, such as cirrhosis, may cause portal hypertension. This refers to high blood pressure in your portal vein. Unlike your other veins, which carry blood to your heart, the portal vein transports blood from your digestive organs to your liver.
Portal hypertension can cause swelling in the small, thin blood vessels around your esophagus that connect to your liver. These enlarged blood vessels are called varices. Without treatment, varices may rupture, resulting in severe bleeding.
A procedure called variceal banding, or endoscopic band ligation, uses tiny elastic bands to treat ruptured varices and
Ruptured esophageal varices are the
Symptoms of ruptured varices include:
- vomiting blood
- passing black or bloody stools
- feeling lightheaded or fainting
If you think you may have ruptured varices, seek immediate medical attention.
Endoscopic variceal banding is the
Variceal banding ties off the varices, preventing them from bleeding.
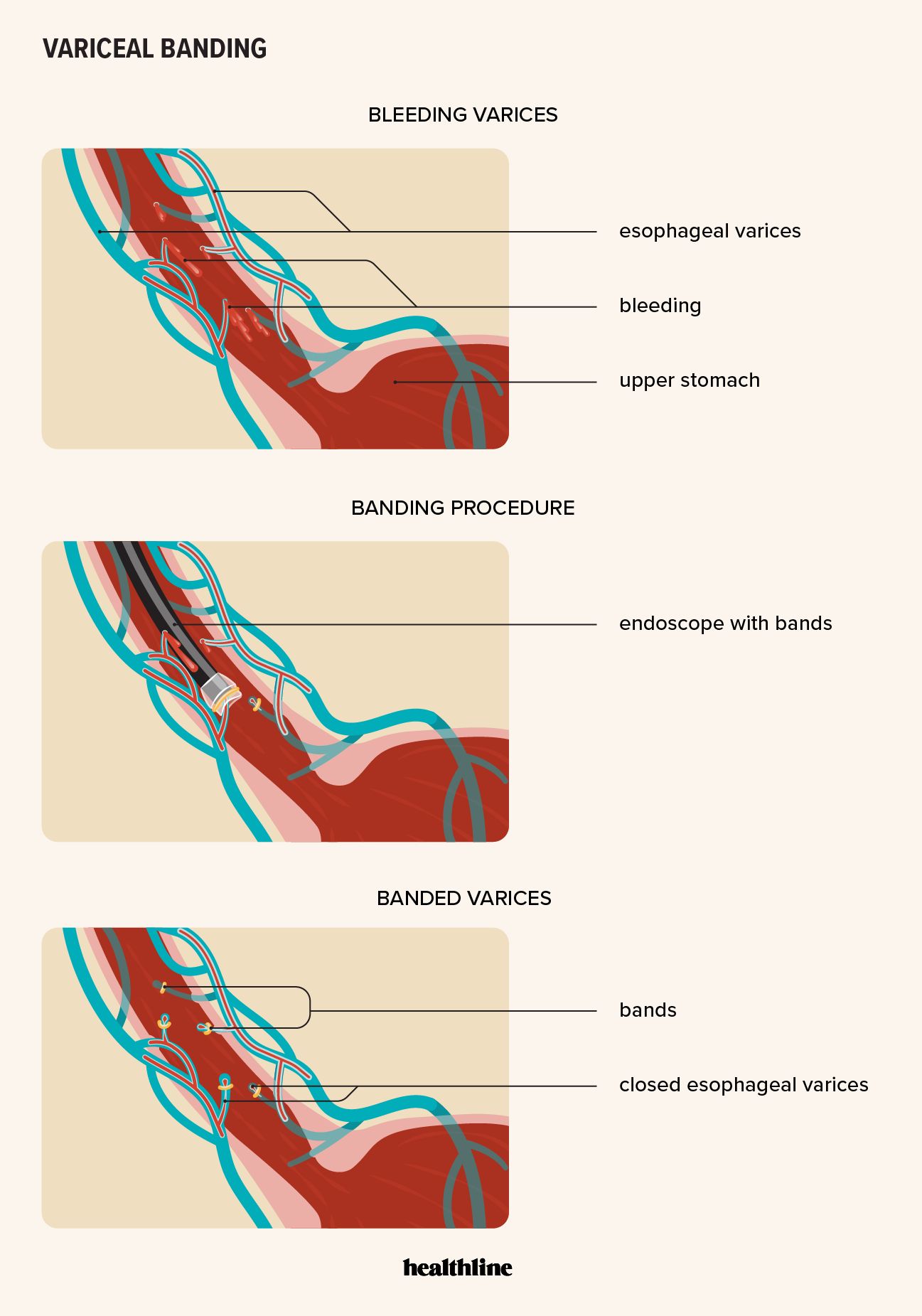
Doctors perform variceal banding via an upper endoscopy. They place tiny elastic bands around the varices using an endoscope, which is a thin, flexible tube with a light and camera on one end.
The doctor will advise you about how to prepare for variceal banding. You may need to fast for up to 12 hours before the procedure and stop taking prescribed or over-the-counter medications, such as aspirin or blood thinners.
A healthcare professional (HCP) will give you a sedative through an intravenous injection, so you’ll need someone to take you home afterward. The HCP may spray your throat with a local anesthetic to prevent you from gagging when the endoscope is inserted. They’ll also use a mouth guard to prevent any damage to your teeth or gums.
The doctor will then load small elastic bands into a specialized banding device inside the endoscope. As you lie on your side on the exam table, the doctor will insert the endoscope into your mouth and down your throat.
The endoscope’s camera sends video to a monitor so that the doctor can see your esophagus up close.
When the endoscope reaches the varices, the doctor will apply suction, pulling the varices into the banding device. They’ll then wrap an elastic band around each gathered vein, cutting off its blood supply.
The doctor will wrap any bleeding varices first, then move on to the other varices. They’ll then remove the endoscope.
Vertical banding is generally a safe procedure. There is a small risk of the following complications:
- tears to the esophagus
- bleeding
- an adverse reaction to the sedative, such as heart or breathing problems
Your doctor may advise you not to eat or drink for 2 hours after the banding.
You should also avoid any strenuous activities for about 24 hours. Don’t drive until the sedative wears off.
Your throat may feel sore or irritated for a day or two after the procedure, and you may have mild to moderate chest pain.
Pain after variceal banding
According to a 2016 study, about
A
However, some people may need variceal banding every few weeks until the varices are gone or so small that they prevent further bleeding.
A 2016 study of 174 people who had emergency variceal banding found that
A doctor may recommend an upper endoscopy after 6–12 months to see if varices have reoccurred. They may also prescribe beta-blockers to help reduce your portal hypertension.
Other treatment options for esophageal varices include:
- Beta-blockers: Beta-blockers such as nadolol (Corgard) and propranolol (Inderal) lower the blood pressure in your portal vein.
- Endoscopic sclerotherapy: A doctor uses an endoscope to inject a medication into your varices, reducing the swelling.
- Transjugular intrahepatic portosystemic shunt (TIPS): During a TIPS procedure, a doctor inserts a small tube that connects your portal vein to your hepatic vein.
- Distal splenorenal shunt procedure: A doctor separates the vein from your spleen from your portal vein and attaches it to the vein in your left kidney.
The following are the answers to some frequently asked questions about variceal banding.
What is the success rate of banding esophageal varices?
Experts consider variceal banding the most effective procedure for preventing ruptures. It has a success rate of 85–94%.
How long do esophageal varices bands last?
The elastic bands placed around varices generally fall off from
Do varices bands fall off?
Although the bands usually fall off, in
Variceal esophageal banding is a safe and effective way to prevent and treat bleeding varices. This is a complication of advanced liver conditions that can be fatal.
Most people have no further bleeding after their first procedure, but some may need to repeat variceal banding a few times to remove reoccurring varices.
