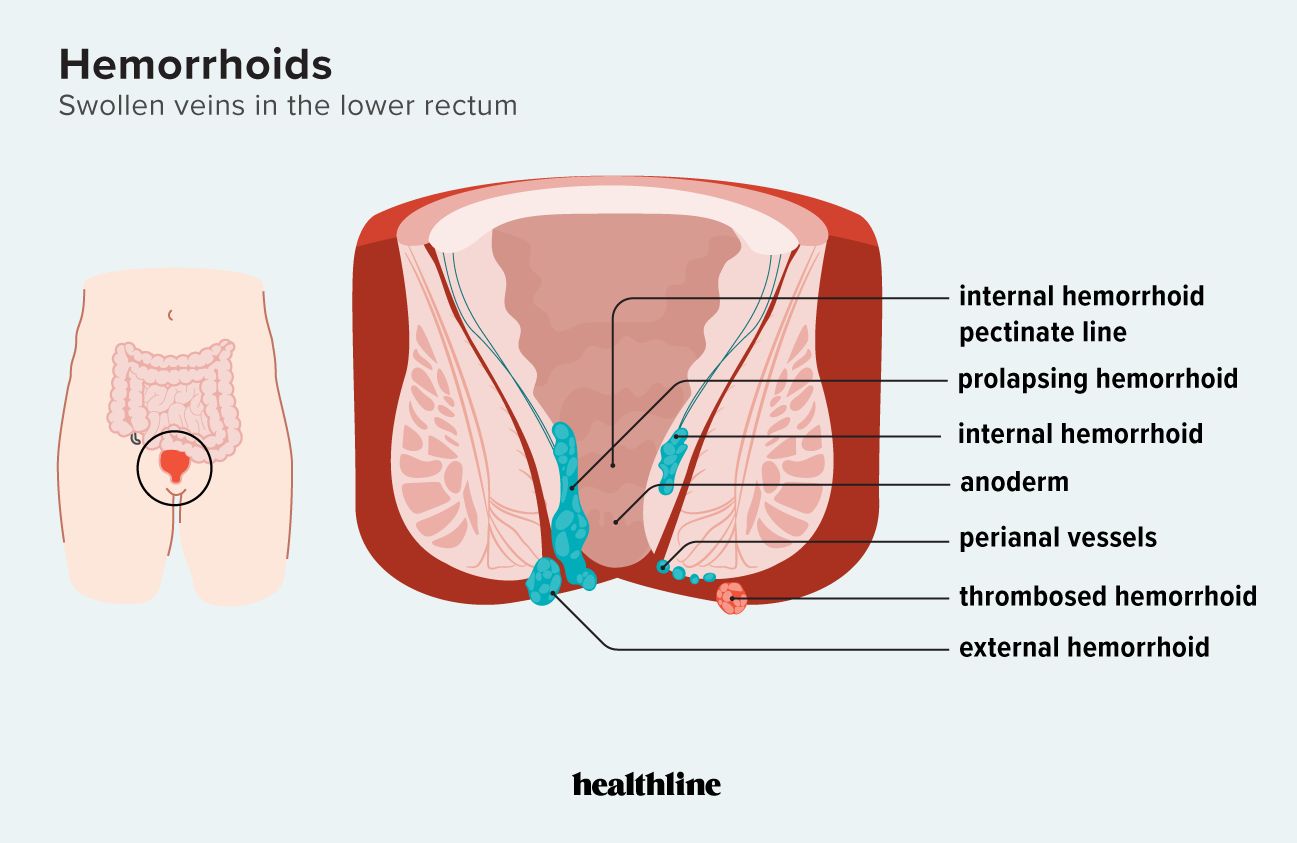
Hemorrhoids can occur on the inside or outside of the rectum. They may also protrude from the rectum and retract when the swelling goes down. Treatment can depend on the severity.
Hemorrhoids, also called piles, happen when clusters of veins in your rectum or anus get swollen (or dilated).
When these veins swell, blood pools inside and causes the veins to expand outward into the membranes around your rectal and anal tissue. This can become uncomfortable or painful.
Hemorrhoids affect
There are four types of hemorrhoids:
- internal
- external
- prolapsed
- thrombosed
Keep reading to learn more about the different types of hemorrhoids, what they look like, and how they’re treated.
Hemorrhoids aren’t always visible. Internal hemorrhoids are found inside your rectum. They’re normally not serious and tend to go away on their own.
There aren’t any nerves that detect pain in your rectum, so you may not always notice internal hemorrhoids. But they can cause symptoms if they grow larger,
- pain or discomfort
- itching
- burning
- rectal bleeding
- mucus in stool
- noticeable lumps or swelling near your anus
A prolapsed hemorrhoid occurs when internal hemorrhoids swell and stick out of your anus. They look like swollen red lumps or bumps. You may be able to see them if you use a mirror to examine this area.
A doctor may
- Grade 1: Not prolapsed at all.
- Grade 2: Prolapsed, but will retract by itself. These may only prolapse when you put pressure on your anal or rectal area, like by straining when you have a bowel movement, and then return to their regular position afterward.
- Grade 3: Prolapsed, and you have to push it back in yourself. These may need to be treated so they don’t become too painful or bleed.
- Grade 4: Prolapsed, and you can’t push it back in without a lot of pain. These usually need to be treated to prevent pain, discomfort, or further complications.
Prolapsed hemorrhoids may have no other symptom than the protrusion, or they may cause pain or discomfort, itchiness, or burning.
In some cases, you may need surgical treatment to remove or correct a prolapsed hemorrhoid so that they don’t cause you any pain or complications.
External hemorrhoids occur on or around your anus. They’re not always visible but sometimes form lumps on the anal surface.
Symptoms are typically the same as those of internal hemorrhoids.
However, you may feel more pain or discomfort when you sit down, do physical activities, or have a bowel movement because external hemorrhoids are located on the outside of your rectal area.
They’re also easier to see when they swell, and the bluish color of the dilated veins is visible beneath the anal skin surface.
A thrombosed hemorrhoid is a hemorrhoid complication in which a blood clot (thrombosis)
Blood clots can happen in both internal and external hemorrhoids. Symptoms may include:
- intense pain and itchiness
- swelling
- skin discoloration, such as a bluish color around the affected area
Speak with a doctor if you experience increasing pain, itchiness, or inflammation around your rectal and anal area. Thrombosed hemorrhoids need to be treated within 72 hours. Otherwise, the clot will start to break, and surgery will no longer be an option. If this occurs, you may have to wait for it to heal on its own.
Speak with a healthcare professional if a hemorrhoid causes pain or discomfort that doesn’t go away after 7 days.
Seek emergency medical attention if your rectal pain is severe or accompanied by the following symptoms:
- fever
- persistent rectal bleeding
- pus in hemorrhoids
- mucus in stool
A doctor may perform several tests to examine the anal or rectal area for hemorrhoids, including:
- physical exam of your rectal area
- finger exam, which involves inserting a gloved finger into the area to check for internal hemorrhoids
- anoscopy
- sigmoidoscopy
These could help a doctor determine the cause of your symptoms and the type of hemorrhoid you have.
Treatment for hemorrhoids depends on the type, degree of prolapse, and severity of your symptoms.
Your treatment plan may include a combination of:
- over-the-counter (OTC) topical creams, gels, and ointments
- OTC medications, such as pain relievers and nonsteroidal anti-inflammatory drugs (NSAIDs)
- home remedies, such as using a cold compress or taking a sitz bath
In some cases, hemorrhoids need to be removed to prevent pain and long-term complications. Some procedures for removal include:
- rubber band ligation
- sclerotherapy
- infrared coagulation
- hemorrhoidectomy
- hemorrhoidopexy
How do you know if it’s a hemorrhoid or not?
Hemorrhoids are not always visible, but they may appear as small lumps inside or outside your anus. Other symptoms of hemorrhoids include discomfort, burning, itchiness, or pain in your rectal area.
What can be mistaken for a hemorrhoid?
Sometimes, symptoms like rectal pain, itchiness, and pain during bowel movements may be due to other conditions,
A healthcare professional can provide a proper diagnosis and treatment plan for you.
Do hemorrhoids go away by themselves?
Hemorrhoids usually go away on their own. However, you may require medical treatment if you experience complications or they don’t go away.
What do bad hemorrhoids look like?
Prolapsed and thrombosed hemorrhoids may appear like swollen lumps with discoloration, blood, and mucus. If you experience this, it’s important to get medical attention to prevent any complications.
Hemorrhoids can be uncomfortable or even painful, but most of the time, you won’t experience any noticeable symptoms.
Internal or external hemorrhoids are likely to heal without causing any symptoms or complications. Prolapsed and thrombosed hemorrhoids are more likely to cause discomfort or increase your risk of complications.
Speak with a healthcare professional if you experience hemorrhoid symptoms. They could provide a diagnosis of the type and an appropriate treatment plan.