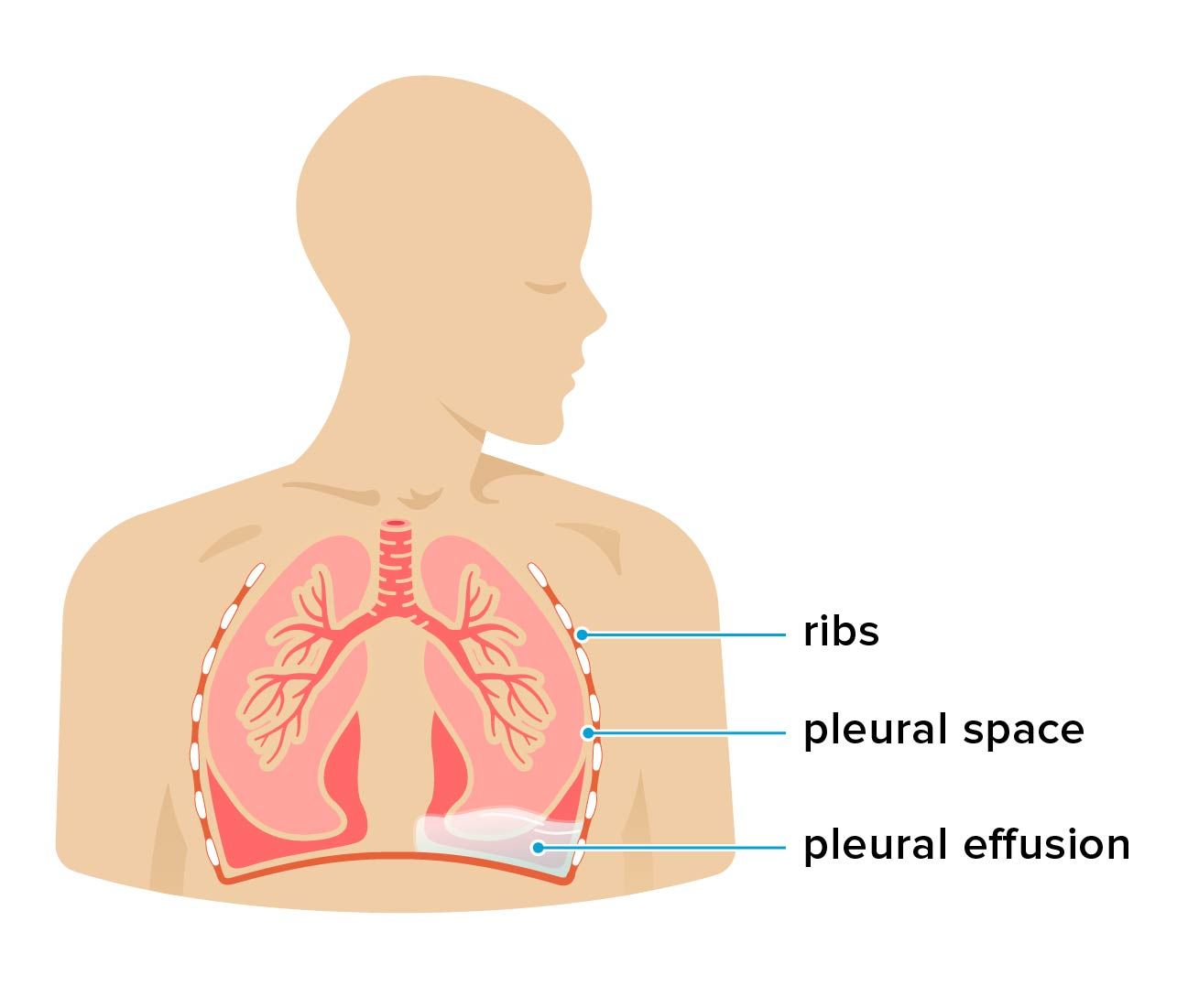
Hepatic hydrothorax is a respiratory condition that affects people with cirrhosis and other serious liver issues. It occurs when fluid builds up in the pleural space.
Hepatic hydrothorax is a complication of advanced liver disease. “Hepatic” describes a condition related to the liver. “Hydrothorax” refers to water buildup in your chest, also known as the thorax.
Hepatic hydrothorax is a type of pleural effusion. This name refers to the specific location of water buildup, known as the pleural space. The pleural space is a cavity that surrounds your lungs, allowing them to expand and contract.
Many health conditions can cause a pleural effusion. Liver conditions are one of the rarer causes. Let’s cover the symptoms, causes, and risk factors for hepatic hydrothorax.
Hepatic hydrothorax typically affects people who have advanced cirrhosis.
Not everyone experiences signs and symptoms. But when symptoms do occur, they resemble a number of other respiratory conditions.
Symptoms of hepatic hydrothorax can include:
- abdominal swelling
- dry cough
- fever or chills
- hiccups
- nausea
- sharp chest pain
- shortness of breath
- low oxygen (hypoxemia)
Cirrhosis is a complication of advanced liver disease that causes severe scarring and makes it hard for your liver to function normally. Liver dysfunction can eventually lead to lung conditions.
There are several theories as to why hepatic hydrothorax develops, according to a
Ascites occurs when liver dysfunction causes fluid to accumulate in your abdominal cavity. This fluid may then move through small gaps in the right side of your diaphragm and into the pleural space. This leads to pleural effusion.
Along with ascites, other risk factors for hepatic hydrothorax in people with cirrhosis include portal hypertension and end-stage liver disease.
People who have hepatic hydrothorax are at an increased risk of life-threatening complications, including:
- blood in the pleural cavity (hemothorax)
- collapsed lung (pneumothorax)
- empyema
- kidney failure
- liver failure
- pleural infection
- pneumonia
- respiratory failure
Doctors use a procedure called thoracentesis to diagnose hepatic hydrothorax in people who have cirrhosis or other known liver conditions.
A doctor might start by taking a chest X-ray or ultrasound to determine the location of the fluid. During thoracentesis, a doctor will use a syringe to extract fluid from your pleural space. The sample is then analyzed for the presence of thin, watery substances called transudate and exudate to confirm the source of the effusion.
Your doctor might also conduct additional imaging scans to rule out other potential causes of a pleural effusion.
There are several available treatments for hepatic hydrothorax. First-line treatments include a low-salt diet and diuretics to reduce water retention.
According to a 2018 review, many people continue to experience symptoms even after adapting their diet and taking medication. When this happens, additional treatments may include:
- Thoracentesis: Thoracentesis is sometimes used to remove excess fluid from the pleural space, which may temporarily relieve symptoms.
- Indwelling tunneled pleural catheter: This treatment involves the placement of a silicone tube to drain pleural fluid and make it easier to breathe.
- Transjugular intrahepatic portosystemic shunt (TIPS): TIPS helps treat portal hypertension, an important risk factor for hepatic hydrothorax. It may reduce fluid buildup in yourd chest.
- Pleurodesis: This procedure involves inserting a chemical substance to make the outside of your lung stick to the inner wall of your chest and prevent fluid from accumulating there.
- Paracentesis: Paracentesis can be used to decrease ascites, which may also reduce the amount of fluid that crosses the diaphragm into the pleural space.
- Liver transplant: When other treatments aren’t successful, liver transplantation might be an option.
Your doctor will thoroughly review your treatment options with you, including the risks and benefits of each procedure.
Hepatic hydrothorax affects approximately
- avoiding alcoholic drinks
- eating a balanced diet
- reducing your salt intake
- maintaining a healthy weight
- seeing your doctor for regular checkups
- managing hepatitis or other liver conditions
If you have cirrhosis, you should call 911 or local emergency services if you experience:
- chest pain
- fever or chills
- shortness of breath
These can be signs of hepatic hydrothorax or another serious condition.
If you already have a hepatic hydrothorax diagnosis, you should see a doctor if your symptoms reappear or worsen while you’re undergoing treatment.
Hepatic hydrothorax can significantly reduce life expectancy for those living with cirrhosis. According to a
The authors of a 2022 cohort study of 942 people who had cirrhosis with ascites found that those who developed hepatic hydrothorax had a fourfold increase in mortality.
Here are some common questions about hepatic hydrothorax.
What is the most common cause of hydrothorax?
The
Can you have hepatic hydrothorax without ascites?
Although hepatic hydrothorax is more common in people with ascites, it can develop in people who don’t show any outward signs of abdominal fluid buildup.
People who have hepatic hydrothorax may experience respiratory symptoms like shortness of breath, sharp chest pain, and coughing. Some people don’t experience symptoms, though.
If you have cirrhosis, consult a doctor to learn more about preventing and treating complications such as ascites, portal hypertension, and hepatic hydrothorax.

