Congestive heart failure (CHF) typically progresses through four stages, with varying symptoms. Your stage may influence your treatment approach and life expectancy.
CHF is a medical condition in which your heart isn’t able to pump blood efficiently. It can result from various underlying heart conditions, such as coronary artery disease, and can lead to fluid buildup in or around the lungs.
The American College of Cardiology (ACC) and American Heart Association (AHA) categorize heart failure into
- specific symptoms
- levels of heart dysfunction
- functional limitations
- overall impact on your quality of life
Read on to learn more about the stages of heart failure and how they influence your treatment options and outlook.
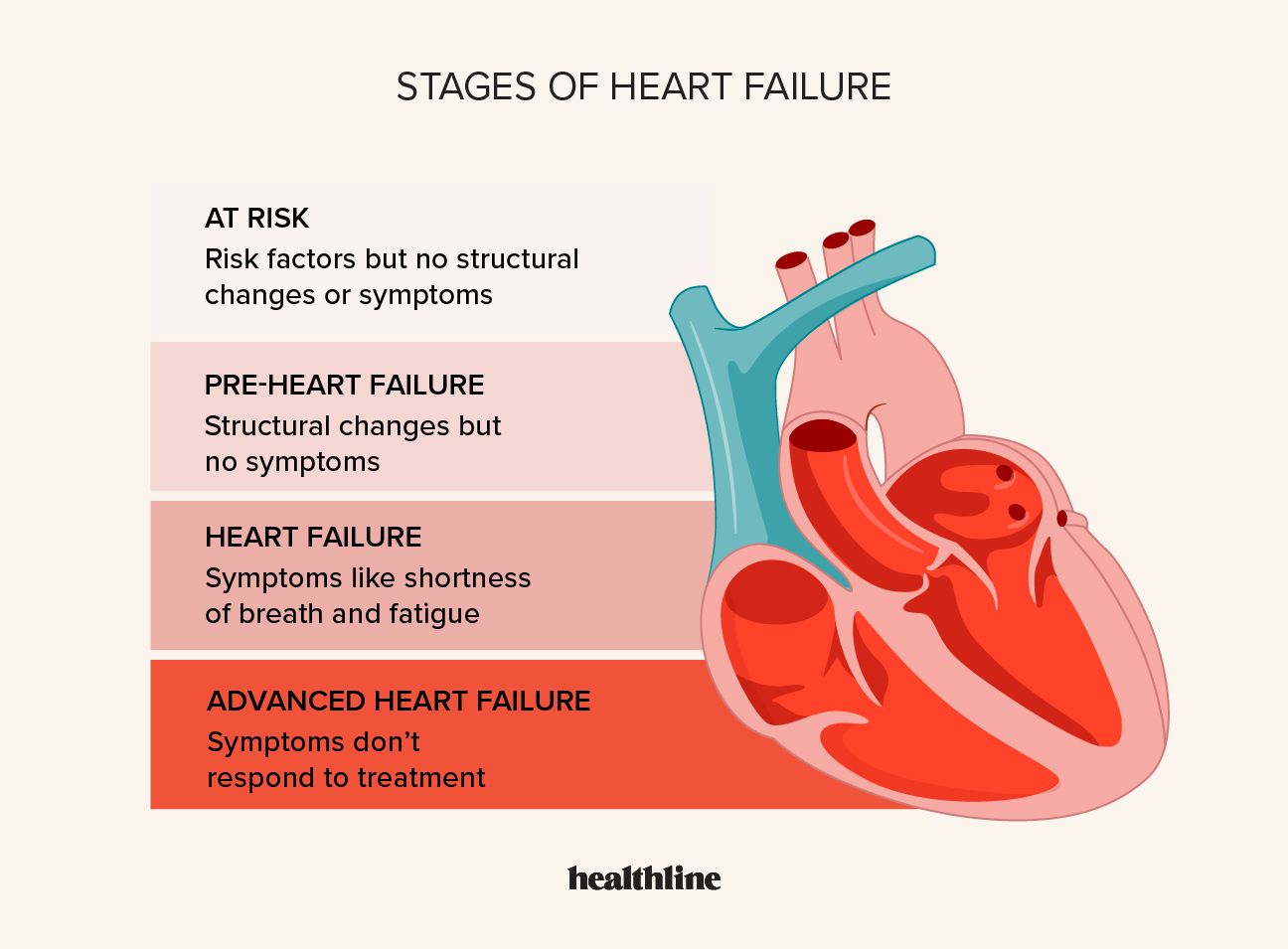
This initial stage is defined by conditions that raise your risk of developing heart failure. You don’t experience any symptoms, and there’s no evidence of structural issues with your heart.
Conditions that can increase your risk may
- hypertension
- diabetes
- obesity
- family history of heart disease
- history of alcohol or substance use disorder
- age over 70
Treatment
Since no symptoms or structural heart changes are present in stage A, the main focus is identifying and managing risk factors. These may include lifestyle changes, such as adopting a healthy diet and exercising regularly to prevent the progression of heart failure.
In the second stage, there should be no symptoms or signs of heart failure. But there’s evidence of at least one of the following:
- structural changes in the heart
- elevated pressure in the left ventricle of the heart
- risk factors from stage A plus elevated B-type natriuretic peptide (BNP) or persistently elevated troponin
Treatment
Stage B treatment aims to manage any underlying structural issues and prevent the development of symptoms. A doctor can prescribe medications like angiotensin converting enzyme (ACE) inhibitors or beta-blockers to improve your heart function and reduce strain on the heart.
This stage is characterized by the onset of symptoms due to heart failure. These symptoms can vary in severity from mild to severe.
They may
- shortness of breath
- fatigue and weakness
- persistent coughing or wheezing
- reduced exercise tolerance
- swelling in the legs, ankles, or abdomen due to fluid retention
- increased heart rate
Treatment
In stage C, treatment aims to manage symptoms. A doctor may prescribe specific medications for heart failure. They may also offer education on heart failure, including fluid and salt restriction.
In stage D, you experience severe symptoms despite receiving appropriate medical treatment. You may experience symptoms even at rest, making it difficult to carry out daily activities. You’re also more likely to experience frequent hospitalizations due to worsening symptoms.
Treatment
Stage D CHF treatment is more aggressive and most often involves referral to an advanced heart failure specialist. They may evaluate you for treatment options such as:
Generally, life expectancy tends to decrease as heart failure progresses from stage A to stage D. People in stage A and stage B, who are at risk or have structural heart irregularities, may have a relatively typical life expectancy with appropriate management.
In stage C, where symptoms are present, life expectancy can vary based on factors such as treatment effectiveness and overall health.
In stage D or advanced heart failure, the life expectancy is shorter, usually between 6–12 months.
Doctors may also categorize CHF according to four classes established by the New York Heart Association (NYHA). These aren’t the same as the four ACC/AHA stages. Still, the
The NYHA classes categorize heart failure based on the physiological impact on your heart’s pumping ability. The four classes are:
| NYHA class | Description |
|---|---|
| I | no physical limitations |
| II | comfortable at rest, but regular activity can cause symptoms |
| III | comfortable at rest, but even light activity can cause symptoms |
| IV | symptoms at rest, with activity causing further discomfort |
Despite their wide use, there’s
CHF can be classified into four stages, A through D. These stages help doctors assess the severity of your condition and guide medical interventions to improve your quality of life. However, identifying symptoms early, following a treatment plan, and making lifestyle changes can significantly influence life expectancy at all stages.
